Varicose veins, those swollen and twisted veins that appear just beneath your skin, often have more than just a cosmetic impact. They can actually significantly affect your quality of life. Let’s take a closer look at the ways varicose veins can impact your daily living.
The following is a breakdown of key areas associated with varicose veins.
- Defining Varicose Veins: These are swollen, twisted veins visible under the skin.
- Symptoms: They’re often painful and can cause severe discomfort.
- Risk Factors: Age, gender, obesity, and family history are all factors.
- Psychological Impact: Varicose veins can lead to self-esteem issues and social anxiety.
- Treatment Options: These range from lifestyle changes to medical procedures.
- Potential Complications: Untreated varicose veins could lead to ulcers or blood clots.
Moving forward, understanding varicose veins and their impact is essential to managing their effects effectively.
A Closer Look at Varicose Veins Impact
Remember, varicose veins are more than just a cosmetic issue. They can significantly affect your overall comfort and quality of life.
If you’re experiencing pain or discomfort from varicose veins, don’t hesitate to seek medical attention.
A variety of treatment options are available, so you don’t have to live with the pain and discomfort associated with varicose veins.
By staying informed about the condition and its potential impacts, you can take steps towards leading a comfortable life.
Defining Varicose Veins
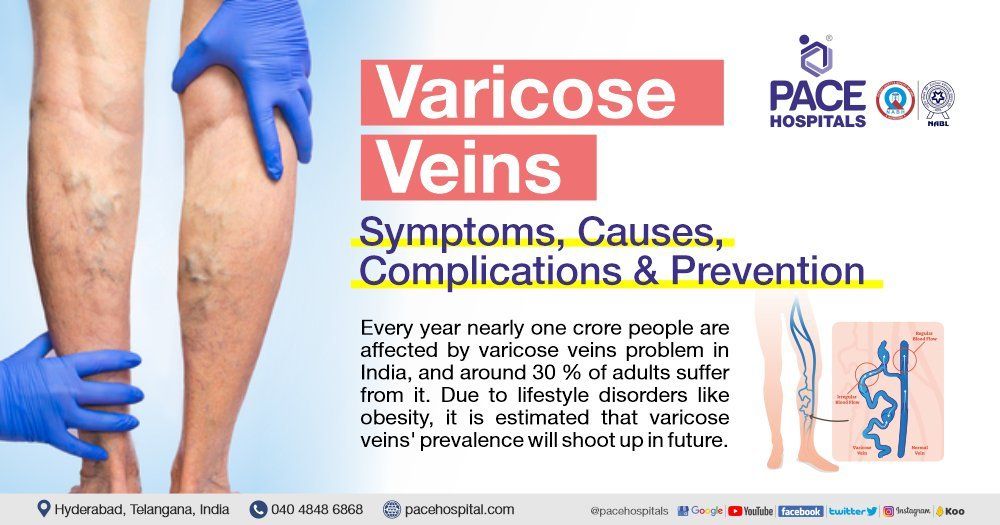
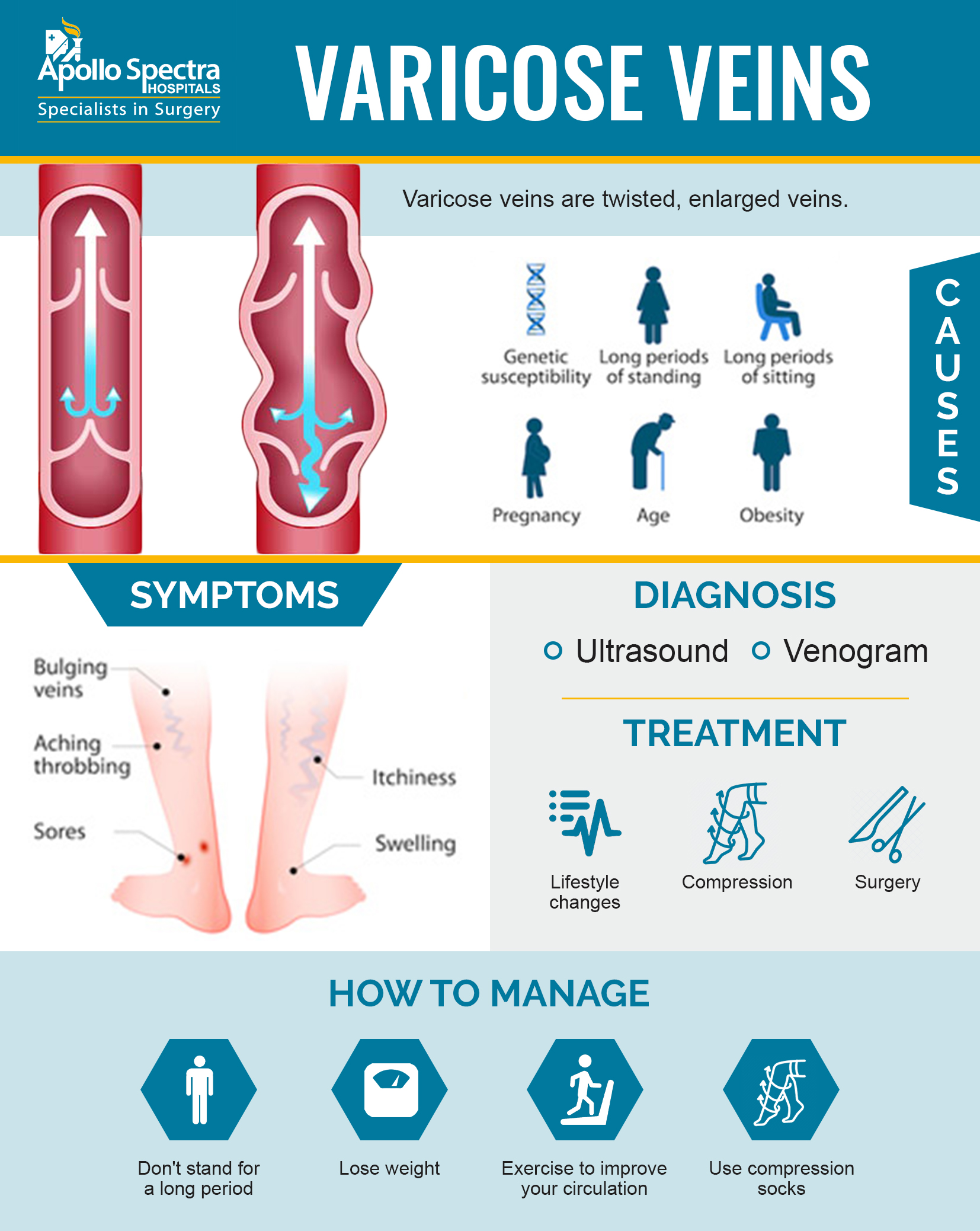
Varicose veins are a common condition, often visible as enlarged, twisted cords beneath the skin surface. They primarily affect the legs and may vary from a minor cosmetic issue to a more severe health concern.
These swollen blood vessels develop due to weakened vein valves that struggle against gravity to return blood to the heart. When these valves fail, blood pools in the veins, expanding them and making them more noticeable on the skin.
- Appearance: Varicose veins can be dark purple, blue, or skin-colored. They have a twisted, bulging appearance, often resembling cords on the legs.
- Symptoms: Although varicose veins might not cause pain, they can result in an achy or heavy feeling in the legs along with burning, throbbing, muscle cramping, and swelling in the lower legs.
- Aggravation: The discomfort tends to worsen after standing or sitting for prolonged periods.
- Itching: Itching around one or more of the veins is another common symptom.
In addition to varicose veins, spider veins can also develop. These are smaller and found closer to the skin’s surface, often resembling a spider’s web. Spider veins can appear on both legs and face.
To understand more about this condition visit Mayo Clinic‘s guide on varicose veins.
Symptoms Associated with Varicose Veins

What are Varicose Veins?
Varicose veins, visible through the skin, are large, twisted, and raised blood vessels. They commonly occur in the legs.
Why do Varicose Veins Form?
The formation of varicose veins is due to weakened vessel walls or faulty valves. This weakening often results in an abnormal twist and turn of these blood vessels.
What Symptoms Indicate the Presence of Varicose Veins?
While some people don’t experience symptoms, others may notice aching pain, heaviness or fatigue in their legs. You may also experience throbbing or burning sensations.
Are Varicose Veins Visually Apparent?
Yes, they can be seen through the skin as blue or dark purple blood vessels. At times, you might also notice hardened veins which feel lumpy to touch.
Is There a Cure for Varicose Veins?
Various treatments are available for varicose veins, including medication and surgical procedures. Lifestyle modifications can also alleviate symptoms.
Are there risks associated with untreated varicose veins?
If left untreated, complications such as skin ulcers or blood clots may arise from varicose veins.
For deeper information on the topic, consider visiting WebMD.
Risk Factors for Varicose Veins

Varicose veins affect numerous individuals worldwide. Understanding the risk factors can help in prevention and management.
Women, due to hormonal changes related to menstruation and pregnancy, are more prone to this condition.
Age is another contributing factor, as older adults are more likely to develop varicose veins, owing to weakening of veins over time.
Heredity can also play a role in varicose vein development. If parents or siblings suffer from it, your risk increases.
| Factors | Risk Increase |
|---|---|
| Pregnancy | High |
| Obesity | Moderate |
| Prolonged Standing/Sitting | Moderate |
| Weak Vein Valves | High |
| Blood Clotting Disorders | Moderate-High |
Details of the table illustrate how different conditions influence the risk of developing varicose veins.
Individuals who stand or sit for extended periods may face an elevated risk due to increased pressure on their veins.
If you have weak vein valves that malfunction or are genetically predisposed to ineffective valves, blood may pool in your veins leading to this condition.
Blood clotting disorders such as deep vein thrombosis are also linked to an increased likelihood of developing varicose veins.
Suffering trauma to the legs or having undergone previous surgery can heighten the risk. Certain medications, like exogenous hormones and birth control pills, are associated with a higher probability of varicose veins as well.
Hormonal changes, increased vein pressure due to factors like tumours or tight clothes, and smoking are additional risk factors. Each has the potential to facilitate the development of varicose veins.
To learn more about varicose veins and their risk factors, visit HealthLine.
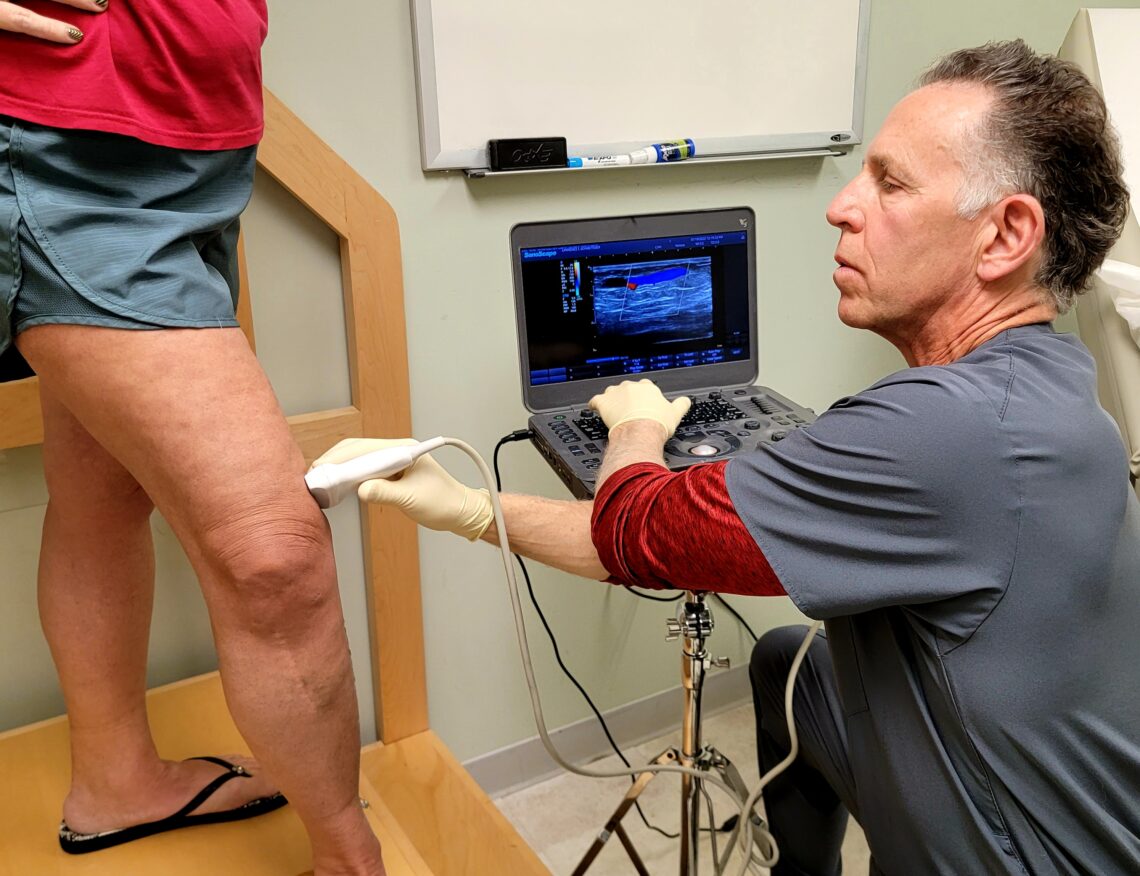
Diagnosis Methods for Varicose Veins
A thorough physical examination forms the initial part of diagnosing varicose veins. Doctors will often inquire about a patient’s family history pertaining to varicose veins and symptom duration.
Physical attributes like height, weight, and overall health conditions are also considered. The presence or expansion of varicose veins and other symptoms are assessed during this phase.
Doctors commonly inspect the veins by palpation, which basically means feeling the veins. They also look out for signs of bleeding or ulcers alongside varicose veins.
The diagnostic process may involve the patient standing for around 5 to 10 minutes as this can make the veins more visible. This aids doctors in evaluating the scope of varicose veins effectively.
The use of duplex ultrasound visualization greatly improves the precision of diagnosis. It helps identify any defective veins that require intervention.
Doppler ultrasound is another tool that can measure blood flow and determine the functioning of valves in both perforating and deeper veins. Such findings are particularly valuable when considering surgical options.
For more information about varicose vein diagnosis, MedicineNet provides comprehensive insights.
The Psychological Impact of Varicose Veins
Varicose veins, a condition affecting mainly women and people who are overweight, have a significant psychological impact. Most patients never or intermittently wear compression stockings.
A large proportion of patients reported that their quality of work was compromised due to this condition, with many resorting to cutting down hours.
Lifestyle Limitations
Furthermore, everyday activities such as standing for long periods become a challenge, with over half of the patients facing some sort of limitation.
Moreover, varicose veins impose restrictions on clothing choices, due to concerns about appearance.
The Role of Symptoms
Interestingly, severity of symptoms did not correlate with vein size but were notably worse for those at advanced stages of the disease.
The level of functional restriction and emotional distress varied directly with symptom scores.
Psychological Implications
An extensive part of the psychological toll was tied to feeling limited in terms of physical ability and becoming overly self-conscious about appearance.(source)
These results highlight the importance of understanding the emotional burden associated with varicose veins.
Treatment Options for Varicose Veins
Nowadays, varicose veins are no longer a lifelong burden. Cutting-edge, minimally invasive treatments provide a ray of hope for many.
These treatments are not only less painful but they are also time-efficient. Most importantly, they promise long-term success when conducted by a seasoned phlebologist.
The advancements in venous disease treatments have allowed countless individuals to live without the pain, discomfort and embarrassment of varicose veins.
It’s vital that venous diseases be managed by specialists – phlebologists. A thorough understanding of the issue and its impact on an individual’s health is crucial.
Your first visit at a vein healthcare center might involve a visual assessment of your legs and an ultrasound mapping of your venous system. This helps the specialist identify areas of concern.
There are two key treatment methods:
- Endovenous Treatments: This category includes treatments like endovenous laser ablation (EVLA) and radio frequency ablation (RFA). These are minimally invasive procedures used to tackle large varicose veins.
- Compression Therapy: This involves wearing graduated compression stockings. These can halt the progression of venous disease, reduce symptoms and minimize clot risk.
Maintaining a healthy lifestyle, regular exercise, and avoiding prolonged stagnancy also play an important role in prevention. Learn more about these treatment options here.
Potential Complications of Varicose Veins
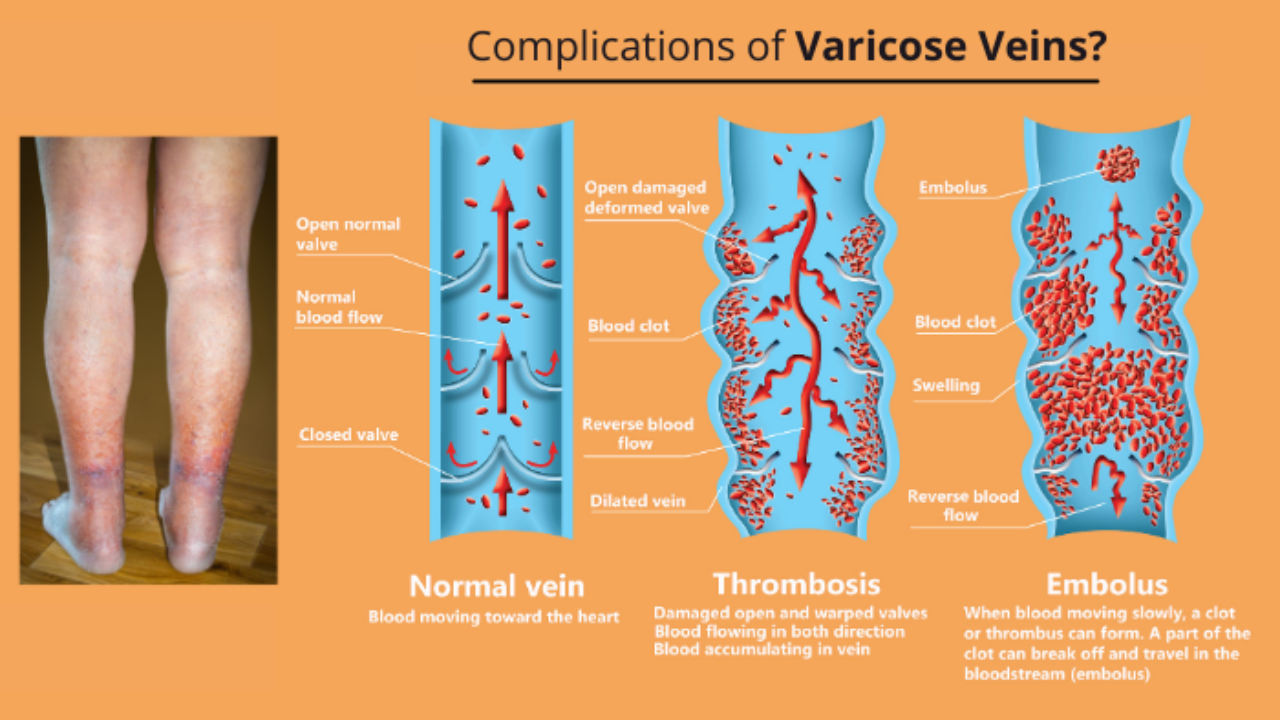
Varicose veins often cause discomfort and may signal more severe health issues.
The complications can range from minor inconveniences to critical, life-threatening conditions.
Understanding these risks helps inform treatment decisions and manage patient expectations.
- Ulcers: These painful skin lesions typically form around the ankles in advanced stages of varicose veins, presenting a significant challenge in terms of treatment.
- Blood Clots: Deep vein thrombosis (DVT) is a serious condition where blood clots form in affected veins. If dislodged, these clots can cause a potentially fatal pulmonary embolism.
- Bleeding: The position of varicose veins close to the skin’s surface can lead to severe bleeding which, if not managed promptly, can be life-threatening.
- Skin Discoloration: Progression of varicose veins can result in a darkening of the skin around the affected area, a change that may be irreversible.
- Pain and Swelling: Flare-ups of varicose veins can cause significant discomfort and swelling, becoming chronic and debilitating over time.
- Superficial Thrombophlebitis: This painful condition occurs when clots form in veins near the skin’s surface.
- Lipodermatosclerosis: This condition happens when fatty tissue beneath the skin becomes inflamed; it is often preceded by chronic venous insufficiency.
American Vein & Vascular Institute is well-trained in addressing these complications. Their registered vascular technologists perform every ultrasound exam to ensure accurate diagnosis and treatment.
For more insights, visit the American Vein & Vascular Institute website.
Addressing varicose veins early and appropriately reduces the risk of experiencing these complications.
Preventive Measures for Varicose Veins
Varicose veins are commonly noticed in individuals assigned female at birth than those assigned male. These swollen, twisted veins can lead to discomfort and health complications if untreated.
Maintaining a healthy lifestyle plays a crucial role in managing varicose veins effectively. Regular exercise and weight management can alleviate symptoms and prevent worsening conditions.
Wearing compression stockings is another preventive measure. It reduces the risk of recurrence post-treatment, aiding in overall vein health.
| Preventive Measures | Benefit | Potential Risk |
|---|---|---|
| Healthy Lifestyle | Alleviates symptoms | Poor management can worsen conditions |
| Regular Exercise | Improves blood flow | Sedentary lifestyle increases risk |
| Use of Compression Stockings | Curtails recurrence post-treatment | Absence can lead to relapse |
| Weight Management | Lowers strain on veins | Obesity elevates risk of varicose veins |
| Pregnancy Care | Limits vein dilation during pregnancy | Lack of care may escalate issues post-pregnancy |
| Regular preventive measures significantly enhance vein health. | ||
In some cases, varicose veins reappear after treatment, particularly with obesity or sedentary lifestyle. Furthermore, they might return in individuals who become pregnant post-treatment.
Sometimes, varicose veins are a normal part of aging, but in other instances, they signify underlying vein issues. Awareness of these symptoms and potential causes can ensure timely intervention and treatment from a vascular specialist.
Life After Varicose Vein Treatment
Undergoing varicose vein treatment such as sclerotherapy can significantly improve the appearance and health of your veins.
This minimally invasive procedure involves injecting a solution into the vein, causing it to contract and eventually fade.
Qualifications for Sclerotherapy
Consulting with a vascular specialist determines eligibility for sclerotherapy. Certain conditions may disqualify some individuals from this treatment.
People with a history of blood clots or specific medical conditions are not typically eligible. However, those on birth control pills can receive sclerotherapy.
The Sclerotherapy Procedure
Sclerotherapy does not require anesthesia, usually takes between 15-30 minutes and is performed in-office.
Patient experiences vary – some may feel mild stinging or cramps upon needle insertion.
Recovery Period Considerations
Most patients resume normal activities immediately after sclerotherapy.
To prevent blood clot formations, frequent walking is recommended post-procedure.
Sclerotherapy Side Effects
While temporary side effects such as bruising and minor skin sores are common, rare occurrences like inflammation around the injection site have been reported.
A source that I found while researching this topic provides more in-depth information on the subject.
When to Seek Medical Attention

If you’re dealing with varicose veins, knowing when to seek medical help is vital. One crucial situation to know about is a case of restricted breathing.
Varicose Veins and Breathing Trouble
Varicose veins can occasionally cause trouble breathing. It’s a symptom that should never be ignored as it might indicate a severe underlying condition.
Another red flag is acute chest discomfort or pain, particularly if it’s persistent. This could signal a cardiovascular issue related to varicose veins.
Chest Pain and Varicose Veins
Chest pain is not common with varicose veins, but if you experience it, don’t delay seeking emergency medical attention.
An unusual headache can also occur in some cases. The onset may be sudden and the pain severe, indicating a need for immediate medical intervention.
Unusual Headaches and Varicose Veins
While varicose veins typically cause pain in the legs, an unusual or severe headache should not be overlooked.
If you suddenly find yourself unable to speak, see, walk, or move, this could be an urgent indication of neurological issues associated with varicose veins.
In instances where confusion sets in suddenly without any apparent reason, immediate medical intervention is necessary as confusion can be an indicator of severe health concerns related to varicose veins.
This MedlinePlus guide provides further details on when to seek urgent care for various medical situations.
Veins’ Mental Toll
Varicose veins do more than harm physical health; they can significantly impact psychological wellness. Often leading to feelings of embarrassment and self-consciousness over their appearance, they can result in social avoidance and even depression. It’s crucial to take into account not just physical pain, but also the emotional distress caused by varicose veins.
